
Your liver plays a critical role in maintaining overall health by filtering toxins, producing bile, storing essential nutrients, and supporting digestion. With the constant exposure to toxins from the environment, food, and alcohol, it’s crucial to support the liver in its detoxification process. The good news is that certain foods can help promote liver health and enhance its natural detoxification abilities. In this article, we will explore the best foods for liver detox and how incorporating them into your diet can help support your liver in flushing out toxins and maintaining optimal function.
Understanding the Role of the Liver in Detoxification
The liver is one of the body’s most vital organs, responsible for detoxifying harmful substances, metabolizing nutrients, and filtering out waste products. It also produces proteins involved in blood clotting and stores important nutrients such as vitamins and minerals. Given its essential functions, it’s important to prioritize liver health and support its natural detoxification processes.
When the liver is overloaded with toxins or damaged, it can struggle to function properly, leading to various health issues such as fatigue, digestive problems, and even liver disease. Fortunately, the liver has a remarkable ability to regenerate itself, and with the right dietary support, you can help boost its detoxification capabilities.
Step 1: The Best Foods for Liver Detox
Incorporating certain nutrient-rich foods into your diet can help support liver health and enhance its detoxification processes. Here are some of the best foods for liver detox that you can include in your daily meals.
Subheading: Top Foods for Liver Health
- Leafy Greens: Vegetables like spinach, kale, and arugula are rich in chlorophyll, which helps remove toxins from the bloodstream and neutralize heavy metals. Leafy greens also contain antioxidants and essential nutrients that support the liver in its detoxification efforts.
- Beets: Beets are a powerful liver detox food because they help increase bile production and improve liver function. The betaine in beets helps the liver break down and eliminate toxins more efficiently, while also supporting the liver’s ability to metabolize fat.
- Garlic: Garlic contains sulfur compounds, which activate liver enzymes responsible for flushing out toxins. It also has high levels of allicin, an antioxidant that protects the liver from oxidative stress and supports detoxification.
- Turmeric: Known for its anti-inflammatory and antioxidant properties, turmeric contains curcumin, which has been shown to help reduce liver inflammation and improve liver enzyme function. It supports the liver’s ability to break down toxins and process fats.
- Grapefruit: Rich in vitamin C and antioxidants like naringenin, grapefruit is a potent liver detox food. It helps stimulate the production of enzymes involved in detoxification, while its high water content also helps keep the liver hydrated, aiding in the elimination of toxins.
- Avocados: Avocados are packed with healthy fats and antioxidants that support liver health. The healthy monounsaturated fats found in avocados help reduce liver inflammation and improve fat metabolism, making it easier for the liver to detoxify.
- Green Tea: Green tea is high in catechins, a type of antioxidant that has been shown to support liver function and improve fat metabolism. Drinking green tea regularly can help protect the liver from damage and support its detoxification process.
- Lemons: Lemons are an excellent source of vitamin C, which supports the production of enzymes that help detoxify the liver. The citrusy fruit also has a cleansing effect on the digestive system, which in turn helps support liver health by reducing the burden of waste on the liver.
- Cruciferous Vegetables: Vegetables such as broccoli, cauliflower, and Brussels sprouts contain compounds that help increase the liver’s production of detoxifying enzymes. These vegetables are rich in fiber and antioxidants, which support liver detoxification and reduce inflammation.
- Walnuts: Walnuts are rich in omega-3 fatty acids and glutathione, both of which help detoxify the liver. They also provide important antioxidants that help protect the liver from oxidative damage and support its cleansing functions.
Incorporating these foods into your daily diet can provide the liver with the nutrients it needs to perform its detoxifying functions more effectively. A balanced diet rich in fruits, vegetables, healthy fats, and antioxidants will keep your liver in optimal health and support its detoxification process.
Step 2: Lifestyle Tips to Support Liver Detox
While eating the best foods for liver detox is essential, maintaining an overall healthy lifestyle is equally important in supporting liver health. Here are some additional lifestyle tips that can help optimize liver function:
Subheading: Lifestyle Habits for Liver Support
- Stay Hydrated: Drinking plenty of water is essential for liver detoxification. Water helps flush out toxins through the kidneys and supports healthy bile production, which is essential for digesting fats and eliminating waste from the liver.
- Exercise Regularly: Regular physical activity helps improve circulation, reduce inflammation, and promote fat metabolism, all of which support liver detoxification. Exercise also helps maintain a healthy weight, reducing the burden on the liver.
- Limit Alcohol Consumption: Excessive alcohol consumption can damage liver cells and impair its detoxification ability. To support liver health, it’s important to drink alcohol in moderation or eliminate it entirely from your diet.
- Avoid Processed Foods: Processed foods that are high in sugar, salt, and unhealthy fats can put a strain on the liver. Try to focus on whole, nutrient-dense foods that support liver function and avoid highly processed and packaged foods that are often loaded with additives and preservatives.
- Get Enough Sleep: Sleep is essential for the body’s detoxification process, including the liver. Aim for 7-9 hours of sleep per night to allow the body to regenerate and cleanse itself from toxins.
- Reduce Stress: Chronic stress can negatively impact liver function by increasing inflammation in the body. Practicing relaxation techniques such as deep breathing, meditation, or yoga can help reduce stress and promote liver health.
By adopting these lifestyle habits in combination with the best foods for liver detox, you can provide comprehensive support for your liver and overall health.
Step 3: Incorporating Liver-Boosting Foods into Your Diet
Now that you’re familiar with some of the best foods for liver detox, it’s important to know how to incorporate them into your daily meals. Here are a few simple and delicious ways to add liver-supportive foods to your diet:
- Green Smoothies: Add leafy greens, lemon, and avocado to your morning smoothies for a liver-boosting start to the day. You can also add a teaspoon of turmeric and a handful of grapes for extra antioxidant benefits.
- Salads: Create nutrient-packed salads with a variety of liver-friendly ingredients, such as spinach, arugula, beets, and walnuts. Top it off with a light olive oil and lemon dressing for added detox support.
- Stir-Fries: Make a quick stir-fry with cruciferous vegetables like broccoli and cauliflower, garlic, and a bit of turmeric. Serve it with quinoa or brown rice for a healthy, liver-supporting meal.
- Herbal Teas: Drink a cup of green tea or dandelion root tea in the morning or after meals to support liver function and improve digestion. You can also add a slice of lemon to your tea for an added boost.
- Roasted Vegetables: Roast a variety of liver-supporting vegetables such as Brussels sprouts, carrots, and sweet potatoes. Add a sprinkle of garlic and turmeric for additional liver-detoxifying benefits.
Incorporating these simple and delicious foods into your meals will help support your liver’s detoxification process and ensure you’re getting the nutrients necessary for optimal liver health.
Conclusion
Supporting your liver’s detoxification process is essential for maintaining overall health and well-being. By incorporating the best foods for liver detox, such as leafy greens, garlic, turmeric, and avocados, you can provide your liver with the nutrients it needs to function optimally. In addition to eating these liver-supportive foods, adopting a healthy lifestyle with regular exercise, hydration, and stress management will further promote liver health and detoxification. With a well-rounded approach, you can support your liver in its natural detoxification process and ensure long-term wellness.





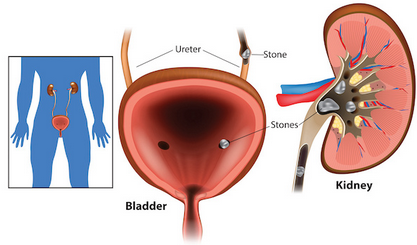 Kidney stones are a common and painful condition that affects millions of people worldwide. These hard mineral deposits form in the kidneys and can lead to severe discomfort when they move through the urinary tract. Understanding how to prevent kidney stones is crucial for maintaining optimal kidney health and avoiding complications. By adopting healthy habits and making informed choices, you can significantly reduce your risk of developing kidney stones.
Kidney stones are a common and painful condition that affects millions of people worldwide. These hard mineral deposits form in the kidneys and can lead to severe discomfort when they move through the urinary tract. Understanding how to prevent kidney stones is crucial for maintaining optimal kidney health and avoiding complications. By adopting healthy habits and making informed choices, you can significantly reduce your risk of developing kidney stones. Living with chronic pain can be a daunting and exhausting challenge, affecting every aspect of life from physical health to emotional well-being. Understanding effective strategies for managing chronic pain can make a significant difference, empowering individuals to regain control and improve their quality of life. Whether you are dealing with pain from a long-term condition or recovering from an injury, finding the right coping mechanisms is essential for relief and resilience.
Living with chronic pain can be a daunting and exhausting challenge, affecting every aspect of life from physical health to emotional well-being. Understanding effective strategies for managing chronic pain can make a significant difference, empowering individuals to regain control and improve their quality of life. Whether you are dealing with pain from a long-term condition or recovering from an injury, finding the right coping mechanisms is essential for relief and resilience.